Pudendal Neuralgia & The Clinical Significance of the Sacrotuberous Ligament
 Sacrotuberous ligament and the pudendal nerve
Sacrotuberous ligament and the pudendal nerve
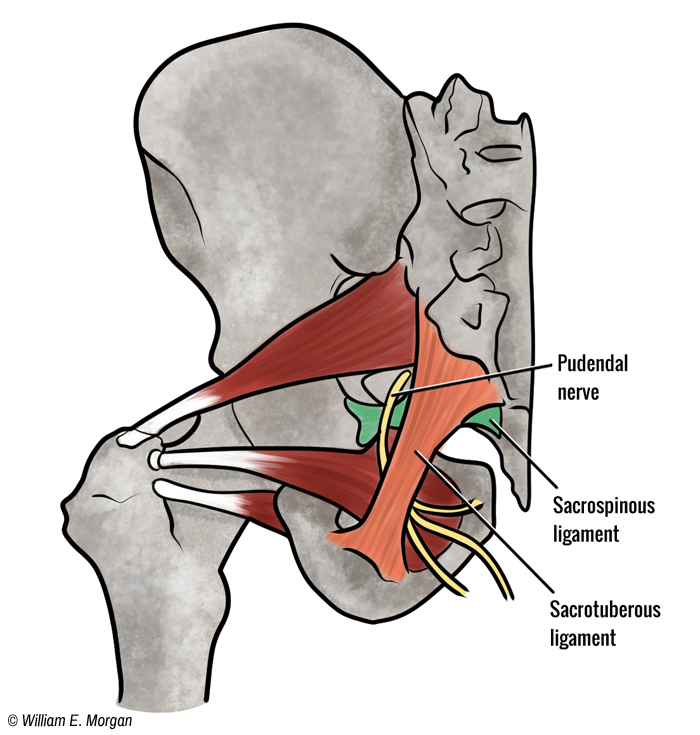
Figure 1. The pudendal nerve travels between the sacrotuberous ligament and the sacrospinous ligament.
To be a master clinician you must become proficient in clinical anatomy, striving to unlock the mysteries of anatomy, optimum human function, and sources of dysfunction. Over the years I have learned that there are certain anatomical crossroads which lend themselves to patterns of dysfunction and injury. Certainly most of us are familiar with some of these anatomic junctions where dysfunctions are common: the carpal tunnel, the piriformis, the thoracic outlet, the iliotibial band, the inguinal ligament, the sacroiliac joint, the plantar fascia , and of course, the spine. Here I will present another clinically significant anatomical juncture, the sacrotuberous ligament, the pudendal nerve, and the sacrospinous ligament.
I was first introduced to the clinical significance of the sacrotuberous ligament and the sacrospinous ligament by my instructor Patrick Montgomery at Palmer-West. Dr. Montgomery was a favorite instructor for most of the students at Palmer. This was due to his very practical clinical knowledge in chiropractic technique. He taught Logan Basic technique at Palmer-west.
Hugh Logan heavily emphasized the treatment of this ligament for patients with spine conditions, not simply for low back pain. He believed a very light and precisely vectored contact on the sacrotuberous ligament would normalize the sacral position and through that, affect the entire spinal column; in fact he believed that other subluxations of the spine to be self-correcting if only the primary sacral subluxation were corrected. While I acknowledge the intent of Dr. Logan’s technique for correcting subluxations, this article will concentrate on using his technique to treat pudendal neuralgia.
The Anatomical Significance of the Sacrotuberous Ligament
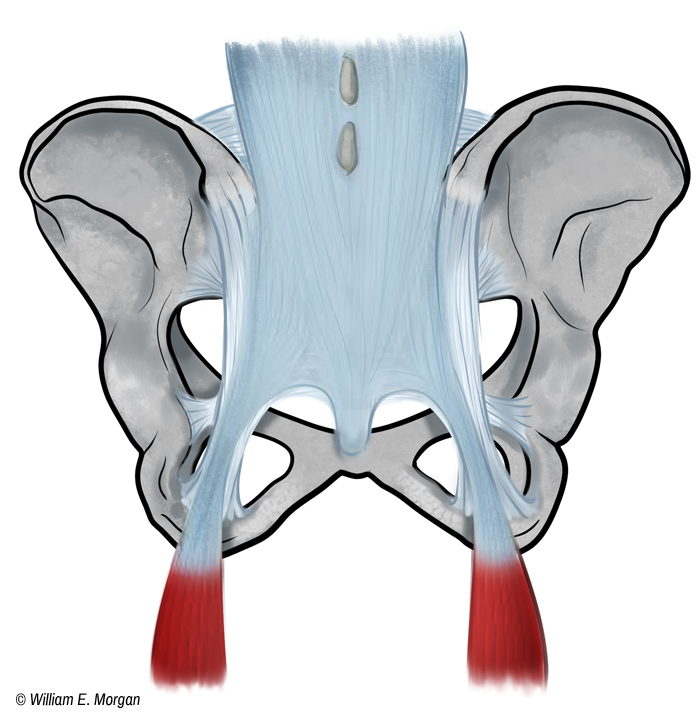
The sacrotuberous ligament arises from the posterior sacrum, and the upper coccyx, with its fibers blending into the complex network of the posterior ligaments of the sacrum connecting this ligament to the posterior superior iliac spine. It extends to the ischial tuberosity. The sacrotuberous ligament contributes to the strength of the pelvis, inhibits nutation, and provides an attachment point for muscles (gluteus maximus and the long head of the biceps femoris). Some fibers of the long head of the biceps femoris attach to the sacrotuberous ligament (sometimes absent in anatomical variants),1 and the inferior fibers of the gluteus maximus attach to it as well. Some authors have credited the biceps femoris with providing an active component to sacroiliac stabilization. While far from providing conclusive evidence, some clinical studies have linked normal hamstring function to the enhancement of sacroiliac stability.2 Additionally, sacroiliac dysfunction has been associated with gluteus maximus weakness.3,4 The sacrotuberous ligament is clearly a significant component in joining the myofascial trains of the lower extremities to the upper body.
Another ligament in this region, the sacrospinous ligament, is deep to the sacrotuberous ligament. It arises from the lateral sacrum and coccyx and attaches to the spine of the ischium (figure 1). Of clinical significance is that the pudendal nerve travels between these two ligaments and can become entrapped.5
 biceps femoris and sacrotuberous ligament
biceps femoris and sacrotuberous ligament
Figure 2. The long head of the biceps femoris blends into the fibers of the sacrotuberous ligament. This provides an active component to the mechanics of pelvic stability and motion. Flexion of the femur or increased tone of the biceps femoris can put tension on the sacroiliac joint.
Pudendal Nerve Entrapment
Pudendal nerve entrapment between the sacrotuberous and sacrospinous ligaments can result in pudendal nerve neuralgia. Pudendal nerve entrapment can result in recurrent pain or numbness of the genitals, rectal pain, reduced awareness of an impending bowl movement, disturbance of normal urination (including overactive bladder), altered sensation during ejaculation, and urinary or bowel incontinence.
Pudendal nerve entrapment can be profoundly life altering, but due to the intimate nature of the symptomatology, many people suffer in silence. Medical treatment for pudendal neuralgia includes pain injections, surgical decompression, and drugs. Chiropractic options include adjustments,6 pelvic floor myofascial treatment, modalities (such as cold lasers), and my preferred method, the Logan Basic Technique.
 Logan Basic Technique
Logan Basic Technique
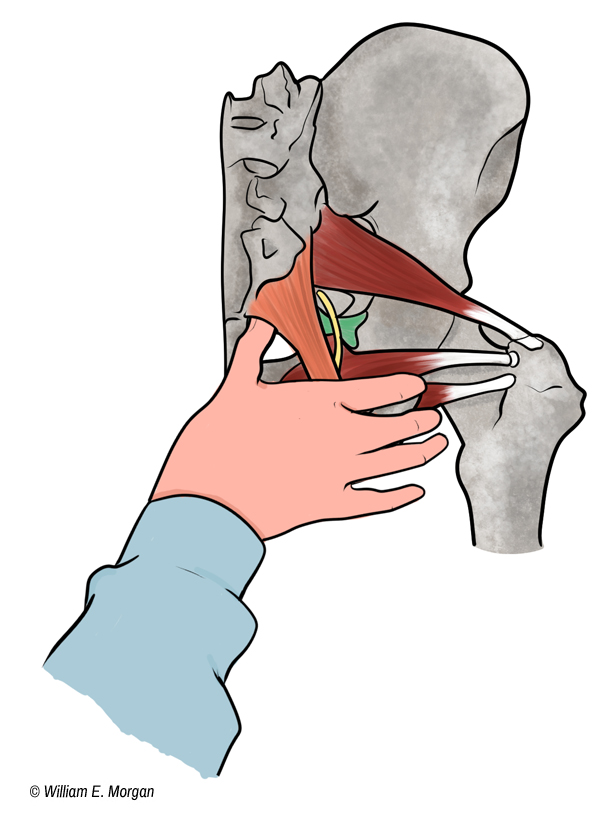
Figure 3. By contacting the anterior portion of the sacrotuberous ligament and applying pressure anterior to posterior and obliquely superior, the ligament can be lifted from the pudendal nerve.
Manual Treatment of the Sacrotuberous Ligament
While I cannot adequately describe all of the specifics, principles, and techniques which comprise Logan Basic Technique in this article, I will share the basic concept of the contact and my adaption of this technique. For a more detailed instruction, I recommend a technique class on the subject.
The patient is positioned in a prone position, flexed slightly at the waist, and at the knees, with any outer restrictive clothing removed. The doctor is contralateral to the side being treated. The doctor palpates to locate the coccyx and then palpates out lateral from the coccyx to find a web-like structure which will feel similar to the web between your fingers. This web is the sacrotuberous ligament. The doctor will then hook the tip of the thumb under the anterior portion of the ligament and distract posteriorly, slightly oblique, and superior. The pressure is light but constant. The direction of pressure can be altered gradually and slightly. While maintaining the contact, the basic technique would have you palpate the paraspinal muscles for feedback to determine when to change the contact or discontinue. I usually perform the contact for 45-60 seconds.
While I would be the first person to admit that the success of this technique is based almost exclusively on clinical outcomes and that there should be more research to validate its success in treating pudendal neuralgia, I would also be the first to tout the numbers of referrals from medical providers at our hospital for treatment of this malady with this technique.
References
1 Vleeming, A., R. Stoeckart, et al. (1989). "The sacrotuberous ligament: a conceptual approach to its dynamic role in stabilizing the sacroiliac joint." Clinical Biomechanics 4(4): 200-203.
2 Cibulka MT, Rose SJ, Delitto A, Sinacore DR. Hamstring muscle strain treated by mobilizing the sacroiliac joint. Phys Ther 1986;66:1220–3.
3 van Wingerden JP, Vleeming A, Buyruk HM, Raissadat K. Stabilization of the sacroiliac joint in vivo: verification of muscular contribution to force closure of the pelvis. Eur Spine J 2004;13:199–205.
4 van Wingerden JP, Vleeming A, Kleinrensink GJ, Stoeckart R. The role of the hamstrings in pelvic and spinal function. Vleeming A, Mooney V, Snijders CJ, Dorman TA, Stoeckart R, editors. editors. Movement, stability and low back pain: the essential role of the pelvis 1997. New York: Churchill Livingstone; 207–10.
5 Marios Loukas,Robert G Louis Jr, Barry Hallner, Ankmalika A Gupta and Dorothy White. (2006) "Anatomical and surgical considerations of the sacrotuberous ligament and its relevance in pudendal nerve entrapment syndrome" Surg Radiol Anat 28(2): 163-169.
6 Cooperstein R, Lisi A, Burd A. Chiropractic management of pubic symphysis shear dysfunction in a patient with overactive bladder. J Chiropr Med. 2014 Jun; 13(2): 81–89.
